Did you know that, for a few minutes after your baby is born, the placenta continues to serve as life support to the baby, with blood continuing to transfer from mom's body through the placenta and umbilical cord into baby? Did you know that allowing that blood to continue transferring to baby can increase blood volume by up to 1/3, thereby benefitting a newborn's lifelong health in significant ways? Yet in the U.S., the protocol in the vast majority of hospitals is to clamp the cord as soon as baby is born.
The World Health Organization (WHO) recommends delaying umbilical cord clamping for a minimum of one minute after a baby is born. Recently, the American Congress of Obstetricians & Gynecologists (ACOG) lengthened their recommendation, now saying to hold off clamping for at least 30-60 seconds post-birth. Many midwives and some OBs promote allowing the cord to stop pulsating before clamping it. You can also read a New York Times article commenting on this new recommendation here.
Why have hospitals historically clamped immediately?
Risk of maternal hemorrhage - Hospitals have routinely clamped immediately after birth with the intention of preventing maternal hemorrhage. However, a growing body of evidence in recent years indicates delaying the clamping some does not increase the risk of hemorrhage
Risk of neonatal jaundice - If baby gets extra blood, they'll get extra bilirubin, which could increase the risk of jaundice due to the fact that newborn livers have a low ability to process bilirubin out of the body efficiently due to an immature liver. However, treatment is readily available in most places (at least in the U.S.), and this is usually an easily treatable condition. For a mom who is breastfeeding, the more frequently she feeds baby, the quicker baby will poop out the bilirubin, thereby decreasing the risk of jaundice.
I want to point out here that the U.S. ranks terribly in maternal health (#61 in the world) and children's well-being (#42nd in the world), and the medical community is trying to find ways to rectify that. The change of recommendation with regard to delayed cord clamping is a small step away from active medical management (i.e., doing things actively to prevent a problem -- things that carry their own risk), toward expectant management (treating a problem only in the unlikely event that it arises).
Even so, research has revealed that hospitals take 15-17 years to change their protocols once evidence-based, revised recommendations are made. (Say whaaaa?! Yes, for real!) So, do not assume that your care provider will automatically default to delayed cord clamping. Always better to have a conversation with your care provider by around 36 weeks of pregnancy to make your request for delayed cord clamping--as well as any other birth preferences--known. I would recommend requesting your ideal, which could be to the longest end of the spectrum -- ie waiting until the blood has stopped flowing and the cord has stopped pulsating. Then you can negotiate down, if needed, based on the comfort level and rationale of your care provider.
Benefits to baby of delayed clamping
Extra blood to the lungs optimally supports baby's respiratory transition from womb to world
Around 3-6 months, many babies become a bit iron-deficient; iron is critical to brain development. Delaying the cord clamping can help prevent this by giving the baby extra iron stores. See this (aforementioned) study, which reports, "improvement in iron stores appeared to persist, with infants in the early cord clamping over twice as likely to be iron deficient at three to six months compared with infants whose cord clamping was delayed."
In this study, 4 year olds who had experience delayed cord clamping showed modestly higher scores in social skills and fine motor skills (though only for boys)
Increases early hemoglobin concentrations (hemoglobin is necessary for carrying oxygen from the lungs to the body's tissues and returning carbon dioxide from the tissues back to the lungs)
Many more benefits have been proven in preemies (also here and here)
Source: nurturingheartsbirthservices.com -- showing time lapse from birth to 15 minutes later.
Common Questions
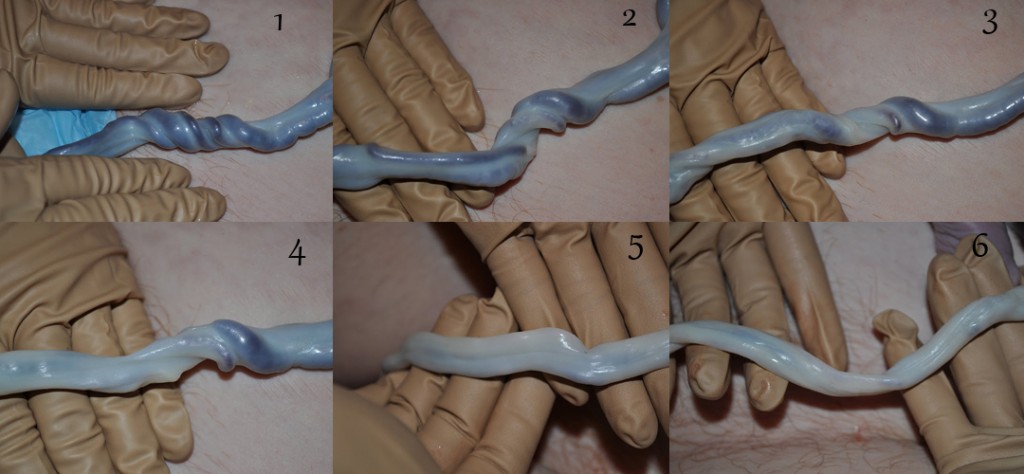
Is it helpful to milk the cord?
You may have heard of "milking" the cord, a way that some care providers try to "expedite" the transferral of blood to baby, there is no evidence this is a recommended alternative. What we are talking about here is leaving nature alone and letting the body, the placenta and the baby do the business of healthy blood transfusion for a few minutes uninterrupted.
If I'm given the scissors to cut my baby's cord, can't I just hold onto them to delay clamping?
No. Since your care provider will first clamp the cord an inch or so out from the belly button and then another inch or two out to stop the flow of blood before the scissors cut the cord.
Is it possible to do both delayed cord clamping and collect for cord blood banking?
The vast majority of care providers will indicate this is not possible, and they are perhaps right, but not necessarily. That is, we have no way of knowing how long the cord will pulsate or how much blood will pump through the cord before the placenta detaches from the uterus and be birthed. Therefore, it would be a gamble to try to delay the clamping and then also try to collect enough blood for cord blood banking. At this point in time, I am of the opinion that--if your care provider can't do both and you have to choose--it's better for babies to receive the blood that belongs to them right at birth (plus, it's free!). That is, unless any of the few known treatable illnesses with cord blood banking run in your family; this could be the exception to the rule.
Conclusion
Delayed cord clamping (waiting at least 1 minute and ideally until the cord has stopped pulsating) is evidence-based and best for your newborn's health. As with most things in birth, we need to do a risk/benefit analysis when deciding which parts of birth need to be medically managed, if any. This is one of many examples that the pendulum historically swung too far in the active/medical management direction and is starting to swing back toward the other--in this case, toward improved global children's health.
Resources
American Congress of Obstetricians & Gynecologists (ACOG) Jan 2017 revised recommendation
"Delayed Umbilical Cord Clamping May Benefit Children Years Later" (NPR)
"Delayed Cord Clamping Should Be Standard Practice in Obstetrics" - Academic OBGYN
"Doctors No Longer Rush to Cut the Umbilical Cord" (New York Times)